Guidelines
With 200 million people affected by peripheral artery disease worldwide and > 600,000 hospital admissions yearly for venous thromboembolic disease in the United States, establishment and adoption of nomenclature for spectral Doppler waveform characterization is essential for communication of disease presence and severity.
Interpretation of Peripheral Arterial and Venous Doppler Waveforms
A Consensus Statement from the Society for Vascular Medicine and Society for Vascular Ultrasound [2020]
https://journals.sagepub.com/doi/10.1177/1358863X20937665Abstract
This expert consensus statement on the interpretation of peripheral arterial and venous spectral Doppler waveforms was jointly commissioned by the Society for Vascular Medicine (SVM) and the Society for Vascular Ultrasound (SVU). The consensus statement proposes a standardized nomenclature for arterial and venous spectral Doppler waveforms using a framework of key major descriptors and additional modifier terms. These key major descriptors and additional modifier terms are presented alongside representative Doppler waveforms, and nomenclature tables provide context by listing previous alternate terms to be replaced by the new major descriptors and modifiers. Finally, the document reviews Doppler waveform alterations with physiologic changes and disease states, provides optimization techniques for waveform acquisition and display, and provides practical guidance for incorporating the proposed nomenclature into the final interpretation report.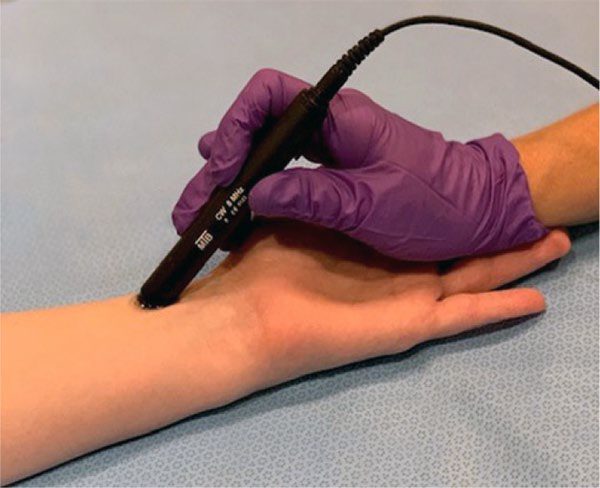
IAC Vascular Testing Communication 2021 Updated Recommendations for Carotid Stenosis Interpretation Criteria
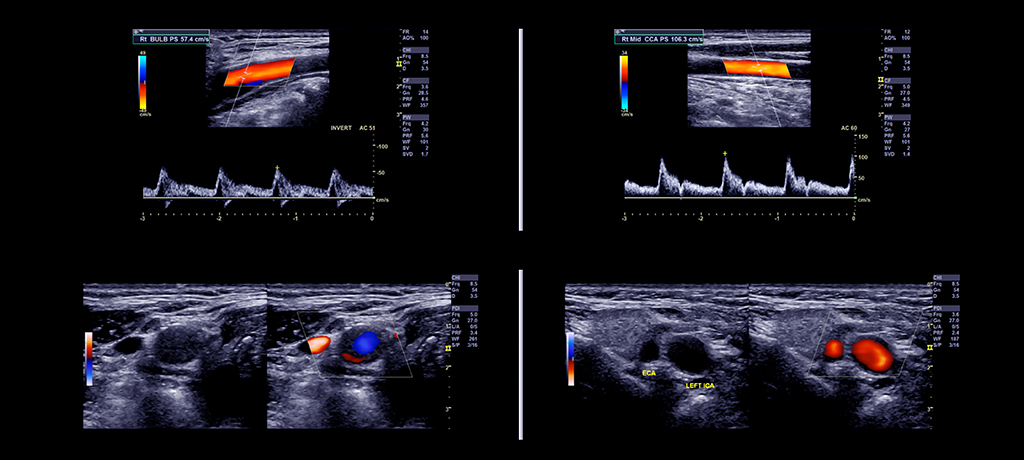
In 2014, IAC Vascular Testing issued a White Paper on the considerable variation in criteria used interpret the degree of internal carotid artery (ICA) stenosis in carotid duplex ultrasound examinations1. In the document, IAC Vascular Testing reviewed the history of the issue and potential impact of this variation on the clinical value and comparability of carotid stenosis measurements. As an initial step to reduce this variability, IAC Vascular Testing recommended adoption of the diagnostic criteria proposed by Society of Radiologists in Ultrasound (SRU) Consensus Conference2 by labs not using validated, internally-derived stenosis criteria. IAC Vascular Testing then developed and carried out a research study using “real world” carotid duplex scans from IAC-accredited vascular labs and contrast arteriography to assess the validity of the SRU Consensus Conference criteria and to potentially refine the SRU criteria or develop distinct criteria that could be applicable to IAC-accredited facilities that perform carotid duplex examinations.
This study was recently completed and the final results have been published in the peer reviewed journal Vascular Medicine3. The data confirmed the findings of several others that the SRU peak systolic velocity (PSV) threshold of 125 cm/sec for a 50% diameter reducing stenosis of the ICA is overly sensitive and has inadequate specificity and accuracy and supports the adoption of a higher PSV threshold value of 180 cm/s. The study sample with high-grade stenoses was insufficient to recommend modification of the SRU Criteria for higher degrees of internal carotid stenosis (70% and 80%). Based upon these data derived from the work product of IAC-accredited labs, IAC Vascular Testing now recommends general adoption of modified SRU criteria incorporating the higher PSV threshold value of 180 cm/sec for 50% diameter reducing ICA stenosis. IAC Vascular Testing recognizes there may be selected cases with 50-69% ICA stenosis in which PSV < 180 cm/sec, but there is elevated ICA/CCA PSV ratio > 2.0 with significant plaque and other features of stenosis (e.g., post-stenotic turbulence). Therefore, all Doppler and gray scale parameters should be considered for the interpretation of the degree of ICA stenosis.
IAC Vascular Testing recommends the use of these modified criteria for carotid interpretation at this time. Broad acceptance of this recommendation will enhance the accuracy of the detection of clinically-relevant ICA stenoses and further reduce the variability in grading of ICA stenosis on duplex studies by IAC-accredited vascular labs.
Recommended Modification of the SRU Consensus Conference Criteria for Internal Carotid Artery Stenosis for Implementation in IAC-Accredited Vascular Laboratories
|
Primary Parameters |
Additional Parameters |
|||
|
Degree of Stenosis, % |
ICA PSV, cm/sec |
Plaque Estimate, % |
ICA/CCA PSV Ratio |
ICA EDV, cm/sec |
|
Normal |
<180 |
None |
<2.0 |
<40 |
|
Normal |
<180 |
None |
<2.0 |
<40 |
|
<50 |
<180 |
<50 |
<2.0 |
<40 |
|
50-69% |
180–230 |
>50 |
2.0–4.0 |
40–100 |
|
>70 but less than near occlusion |
>230 |
>50 |
>4.0 |
>100 |
|
Near occlusion |
High, low, or undetectable |
Visible |
Variable |
Variable |
|
Total occlusion |
Undetectable |
Visible, no detectable lumen |
Not applicable |
Not applicable |
*Plaque estimate (diameter reduction) with grayscale and color Doppler US.
Modified from diagnostic criteria proposed by Society of Radiologists in Ultrasound (SRU) Consensus Conference2
REFERENCES- https://www.intersocietal.org/vascular/forms/IACCarotidCriteriaWhitePaper1-2014.pdf
- Grant EG, Benson CB, Moneta GL, Alexandrov AV, Baker JD, Bluth EI, et al. Carotid artery stenosis: grayscale and Doppler US diagnosis – Society of Radiologists in Ultrasound Consensus Conference. Radiology 2003;229:340-6.
- Gornik HL, Rundek T. Gardener H, et al. Optimization of duplex velocity criteria for diagnosis of internal carotid artery (ICA) stenosis: A report of the Intersocietal Accreditation Commission (IAC) Vascular Testing Division Carotid Diagnostic Criteria Committee. Vascular Medicine 2021; e-published ahead of print. Available for free download at: https://journals.sagepub.com/doi/full/10.1177/1358863X211011253.
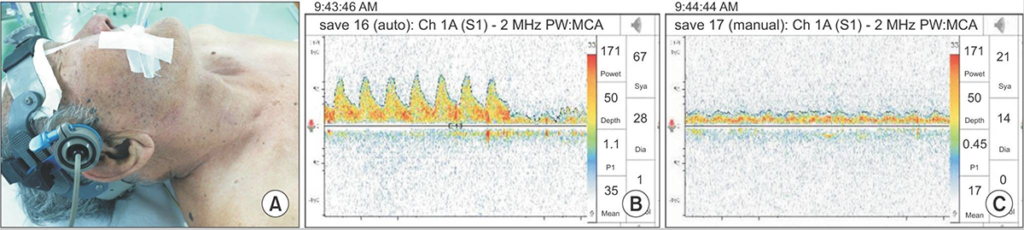
TCD provides a noninvasive and inexpensive (relative to angiography) monitoring modality that can be used in a variety clinical situations ... to provide real-time physiological information that is often unobtainable with other testing without increasing patient risks (repeated radiation doses, contrast injections) and associated costs.
Practice Standards for Transcranial Doppler Ultrasound: Part I—Test Performance
[January 2007]
https://doi.org/10.1111/j.1552-6569.2006.00088.xAbstract
Indications for the clinical use of transcranial Doppler (TCD) continue to expand while scanning protocols and quality of reporting vary between institutions. Based on literature analysis and extensive personal experience, an international expert panel started the development of guidelines for TCD performance, interpretation, and competence. The first part describes complete diagnostic spectral TCD examination for patients with cerebrovascular diseases. Cranial temporal bone windows are used for the detection of the middle cerebral arteries (MCA), anterior cerebral arteries (ACA), posterior cerebral arteries (PCA), C1 segment of the internal carotid arteries (ICA), and collateralization of flow via the anterior (AComA) and posterior (PComA) communicating arteries; orbital windows—for the ophthalmic artery (OA) and ICA siphon; the foraminal window—for the terminal vertebral (VA) and basilar (BA) arteries. Although there is a significant individual variability of the circle of Willis with and without disease, the complete diagnostic TCD examination should include bilateral assessment of the M2 (arbitrarily located at 30-40 mm depth), M1 (40-65 mm) MCA [with M1 MCA mid-point at 50 mm (range 45-55 mm), average length 16 mm (range 5-24 mm), A1 ACA (60-75 mm), C1 ICA (60-70 mm), P1-P2 PCA (average depth 63 mm (range 55-75 mm), AComA (70-80 mm), PComA (58-65 mm), OA (40-50 mm), ICA siphons (55-65 mm), terminal VA (40-75 mm), proximal (75-80), mid (80-90 mm), and distal (90-110 mm) BA]. The distal ICA on the neck (40-60 mm) can be located via submandibular windows to calculate the VMCA/VICA index, or the Lindegaard ratio for vasospasm grading after subarachnoid hemorrhage. Performance goals of diagnostic TCD are to detect and optimize arterial segment-specific spectral waveforms, determine flow direction, measure cerebral blood flow velocities and flow pulsatility in the above-mentioned arteries. These practice standards will assist laboratory accreditation processes by providing a standard scanning protocol with transducer positioning and orientation, depth selection and vessel identification for ultrasound devices equipped with spectral Doppler and power motion Doppler.Practice Standards for Transcranial Doppler (TCD) Ultrasound. Part II. Clinical Indications and Expected Outcomes
[October 2010]
https://doi.org/10.1111/j.1552-6569.2010.00523.xAbstract
Introduction: Transcranial Doppler (TCD) is a physiological ultrasound test with established safety and efficacy. Although imaging devices may be used to depict intracranial flow superimposed on structural visualization, the end-result provided by imaging duplex or nonimaging TCD is sampling physiological flow variables through the spectral waveform assessment. Summary of results: Clinical indications considered by this multidisciplinary panel of experts as established are: sickle cell disease, cerebral ischemia, detection of right-to-left shunts (RLS), subarachnoid hemorrhage, brain death, and periprocedural or surgical monitoring. The following TCD-procedures are performed in routine in- and outpatient clinical practice: complete or partial TCD-examination to detect normal, stenosed, or occluded intracranial vessels, collaterals to locate an arterial obstruction and refine carotid-duplex or noninvasive angiographic findings; vasomotor reactivity testing to identify high-risk patients for first-ever or recurrent stroke; emboli detection to detect, localize, and quantify cerebral embolization in real time; RLS-detection in patients with suspected paradoxical embolism or those considered for shunt closure; monitoring of thrombolysis to facilitate recanalization and detect reocclusion; monitoring of endovascular stenting, carotid endarterectomy, and cardiac surgery to detect perioperative embolism, thrombosis, hypo- and hyperperfusion. Conclusion: By defining the scope of practice, these standards will assist referring and reporting physicians and third parties involved in the process of requesting, evaluating, and acting upon TCD results.Death by neurologic criteria, commonly referred to as brain death, occurs in individuals who have sustained catastrophic brain injury, with no evidence of function of the brain as a whole, a state that must be permanent. The process of this determination always begins with the presumption that the patient does not meet brain death/death by neurologic criteria (BD/DNC), a presumption that must then be disproved. BD/ DNC determination must be accurate and consistent.
Pediatric and Adult Brain Death/Death by Neurologic Criteria Consensus Guideline
Report of the AAN Guidelines Subcommittee, AAP, CNS, and SCCM [October 2023]
http://dx.doi.org/10.1212/WNL.0000000000207740Abstract
Background and Objectives
The purpose of this guideline is to update the 2010 American Academy of Neurology (AAN) brain death/death by neurologic criteria (BD/DNC) guideline for adults and the 2011 American Academy of Pediatrics, Child Neurology Society, and Society of Critical Care Medicine guideline for infants and children and to clarify the BD/DNC determination process by integrating guidance for adults and children into a single guideline. Updates in this guideline include guidance related to conducting the BD/DNC evaluation in the context of extracorporeal membrane oxygenation, targeted temperature management, and primary infratentorial injury.Methods
A panel of experts from multiple medical societies developed BD/DNC recommendations. Because of the lack of high-quality evidence on the subject, a novel, evidence-informed formal consensus process was used. This process relied on the panel experts’ review and detailed knowledge of the literature surrounding BD/DNC to guide the development of preliminary recommendations. Recommendations were formulated and voted on, using a modified Delphi process, according to the 2017 AAN Clinical Practice Guideline Process Manual.Major Recommendations
Eighty-five recommendations were developed on the following: (1) general principles for the BD/DNC evaluation, (2) qualifications to perform BD/DNC evaluations, (3) prerequisites for BD/DNC determination, (4) components of the BD/DNC neurologic examination, (5) apnea testing as part of the BD/DNC evaluation, (6) ancillary testing as part of the BD/DNC evaluation, and (7) special considerations for BD/DNC determination.Despite the severity of the outcomes of PAD in people with diabetes, and particularly for those with DFU, there are few practice guidelines that specifically address the diagnosis and management of PAD in this population. ... This guideline is also part of the IWGDF Guidelines on the prevention and management of diabetes related foot disease. Management of PAD in these people without addressing the other aspects of DFU treatment will frequently result in suboptimal outcomes. The reader is therefore referred to the other IWGDF Guidelines for these aspects.
The 2023 Intersocietal IWGDF, ESVS, SVS Guidelines on Peripheral Artery Disease in People with Diabetes and a Foot Ulcer
https://onlinelibrary.wiley.com/doi/10.1002/dmrr.3686Abstract
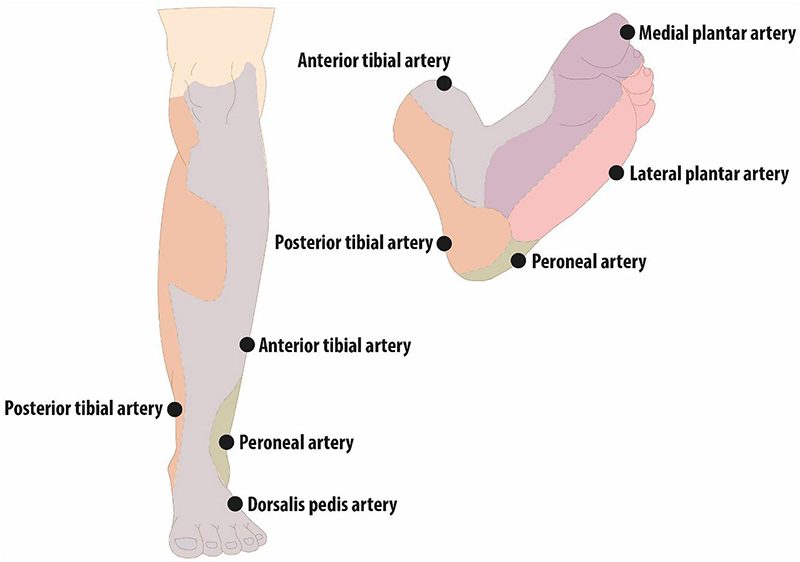
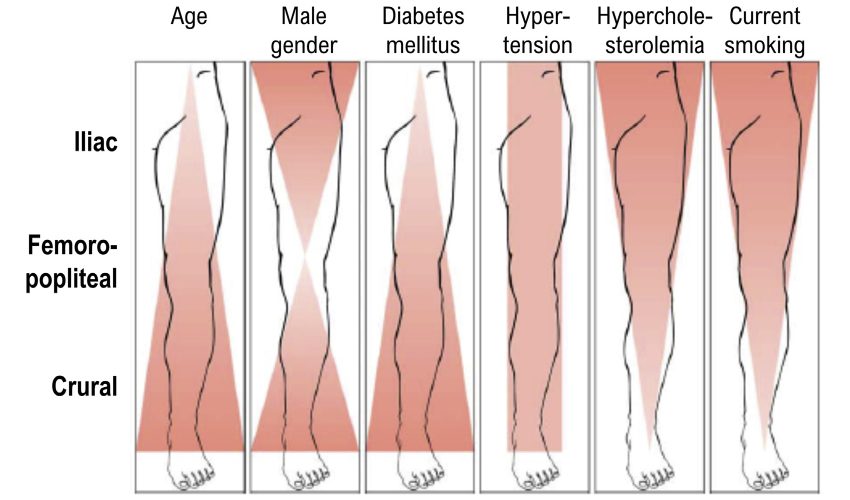
Diabetes related foot complications have become a major cause of morbidity and are implicated in most major and minor amputations globally. Approximately 50% of people with diabetes and a foot ulcer have peripheral artery disease (PAD) and the presence of PAD significantly increases the risk of adverse limb and cardiovascular events. The International Working Group on the Diabetic Foot (IWGDF) has published evidence based guidelines on the management and prevention of diabetes related foot complications since 1999. This guideline is an update of the 2019 IWGDF guideline on the diagnosis, prognosis and management of peripheral artery disease in people with diabetes mellitus and a foot ulcer. For this guideline the IWGDF, the European Society for Vascular Surgery and the Society for Vascular Surgery decided to collaborate to develop a consistent suite of recommendations relevant to clinicians in all countries. This guideline is based on three new systematic reviews. Using the Grading of Recommendations, Assessment, Development, and Evaluation framework clinically relevant questions were formulated, and the literature was systematically reviewed. After assessing the certainty of the evidence, recommendations were formulated which were weighed against the balance of benefits and harms, patient values, feasibility, acceptability, equity, resources required, and when available, costs. Through this process five recommendations were developed for diagnosing PAD in a person with diabetes, with and without a foot ulcer or gangrene. Five recommendations were developed for prognosis relating to estimating likelihood of healing and amputation outcomes in a person with diabetes and a foot ulcer or gangrene. Fifteen recommendations were developed related to PAD treatment encompassing prioritisation of people for revascularisation, the choice of a procedure and post‐surgical care. In addition, the Writing Committee has highlighted key research questions where current evidence is lacking. The Writing Committee believes that following these recommendations will help healthcare professionals to provide better care and will reduce the burden of diabetes related foot complications.
Multiple health care specialists are involved in the management of CLTI, yet lack of public awareness and the frequent failure to make an early diagnosis continue to be major obstacles to effective treatment. Variability in practice patterns is high, contributing to a broad disparity in the use of treatments and clinical outcomes. For example, a study from the United States suggested that many patients do not even receive angiography in the year before major limb amputation.
Global Vascular Guidelines on the Management of Chronic Limb-Threatening Ischemia
Joint guidelines of the Society for Vascular Surgery, European Society for Vascular Surgery, and World Federation of Vascular Societies
https://doi.org/10.1016/j.jvs.2019.02.016Abstract
Chronic limb-threatening ischemia (CLTI) is associated with mortality, amputation, and impaired quality of life. These Global Vascular Guidelines (GVG) are focused on definition, evaluation, and management of CLTI with the goals of improving evidence-based care and highlighting critical research needs. The term CLTI is preferred over critical limb ischemia, as the latter implies threshold values of impaired perfusion rather than a continuum. CLTI is a clinical syndrome defined by the presence of peripheral artery disease (PAD) in combination with rest pain, gangrene, or a lower limb ulceration>2 weeks duration. Venous, traumatic, embolic, and nonatherosclerotic etiologies are excluded. All patients with suspected CLTI should be referred urgently to a vascular specialist. Accurately staging the severity of limb threat is fundamental, and the Society for Vascular Surgery Threatened Limb Classification system, based on grading of Wounds, Ischemia, and foot Infection (WIfI) is endorsed. Objective hemodynamic testing, including toe pressures as the preferred measure, is required to assess CLTI. Evidence-based revascularization (EBR) hinges on three independent axes: Patient risk, Limb severity, and ANatomic complexity (PLAN). Average-risk and high-risk patients are defined by estimated procedural and 2-year all-cause mortality. The GVG proposes a new Global Anatomic Staging System (GLASS), which involves defining a preferred target artery path (TAP) and then estimating limb-based patency (LBP), resulting in three stages of complexity for intervention. The optimal revascularization strategy is also influenced by the availability of autogenous vein for open bypass surgery. Recommendations for EBR are based on best available data, pending level 1 evidence from ongoing trials. Vein bypass may be preferred for average-risk patients with advanced limb threat and high complexity disease, while those with less complex anatomy, intermediate severity limb threat, or high patient risk may be favored for endovascular intervention. All patients with CLTI should be afforded best medical therapy including the use of antithrombotic, lipid-lowering, antihypertensive, and glycemic control agents, as well as counseling on smoking cessation, diet, exercise, and preventive foot care. Following EBR, long-term limb surveillance is advised. The effectiveness of nonrevascularization therapies (eg, spinal stimulation, pneumatic compression, prostanoids, and hyperbaric oxygen) has not been established. Regenerative medicine approaches (eg, cell, gene therapies) for CLTI should be restricted to rigorously conducted randomized clinical trials. The GVG promotes standardization of study designs and end points for clinical trials in CLTI. The importance of multidisciplinary teams and centers of excellence for amputation prevention is stressed as a key health system initiative. (J Vasc Surg 2019;69:3S-125S.)
With all improvements in TCD modalities that includes robotic search and improved monitoring capabilities, this technology in the OR must become regularly employed in the United States. The beneficial effect of a diagnostic test on patient outcome may be considered established if (a) diagnostic studies have shown the test’s ability to detect a particular disorder/abnormality and (b) therapeutic studies have provided evidence on the efficacy of the management of this disorder.
ASNM and ASN Joint Guidelines for Transcranial Doppler Ultrasonic Monitoring: An Update
[February 2022]
https://onlinelibrary.wiley.com/doi/10.1111/jon.13013Abstract
Today, it seems prudent to reconsider how ultrasound technology can be used for providing intraoperative neurophysiologic monitoring that will result in better patient outcomes and decreased length and cost of hospitalization. An extensive and rapidly growing literature suggests that the essential hemodynamic information provided by transcranial Doppler (TCD) ultrasonography neuromonitoring (TCDNM) would provide effective monitoring modality for improving outcomes after different types of vascular, neurosurgical, orthopedic, cardiovascular, and cardiothoracic surgeries and some endovascular interventional or diagnostic procedures, like cardiac catheterization or cerebral angiography. Understanding, avoiding, and preventing peri- or postoperative complications, including neurological deficits following above mentioned surgeries, endovascular intervention, or diagnostic procedures, represents an area of great public and economic benefit for society, especially considering the aging population. The American Society of Neurophysiologic Monitoring and American Society of Neuroimaging Guidelines Committees formed a joint task force and developed updated guidelines to assist in the use of TCDNM in the surgical and intensive care settings. Specifically, these guidelines define (1) the objectives of TCD monitoring; (2) the responsibilities and behaviors of the neurosonographer during monitoring; (3) instrumentation and acquisition parameters; (4) safety considerations; (5) contemporary rationale for TCDNM; (6) TCDNM perspectives; and (7) major recommendations.
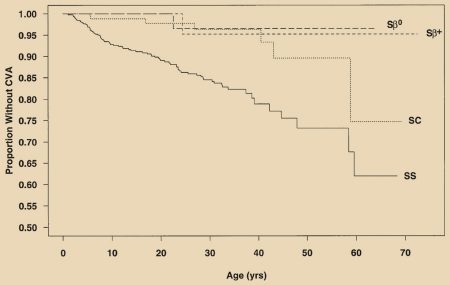
Applying the results of the Optimizing Primary Stroke Prevention in Sickle Cell Anemia Trial (STOP) has contributed to one of the greatest advances in management of SCD. TCD screening coupled with regular blood transfusion therapy for those with an abnormal TAMMV TCDmeasurement is associatedwith a 92% reduction in stroke incidence compared with observation alone.
American Society of Hematology 2020 Guidelines for Sickle Cell Disease Prevention, Diagnosis, and Treatment of Cerebrovascular Disease in Children and Adults
https://doi.org/10.1182/bloodadvances.2019001142Abstract
Background: Central nervous system (CNS) complications are among the most common, devastating sequelae of sickle cell disease (SCD) occurring throughout the lifespan.
Objective: These evidence-based guidelines of the American Society of Hematology are intended to support the SCD community in decisions about prevention, diagnosis, and treatment of the most common neurological morbidities in SCD.
Methods: The Mayo Evidence-Based Practice Research Program supported the guideline development process, including updating or performing systematic evidence reviews. The panel used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, including GRADE evidence-to-decision frameworks, to assess evidence and make recommendations.
Results: The panel placed a higher value on maintaining cognitive function than on being alive with significantly less than baseline cognitive function. The panel developed 19 recommendations with evidence-based strategies to prevent, diagnose, and treat CNS complications of SCD in low-middle– and high-income settings.>/p>
Conclusions: Three of 19 recommendations immediately impact clinical care. These recommendations include: use of transcranial Doppler ultrasound screening and hydroxyurea for primary stroke prevention in children with hemoglobin SS (HbSS) and hemoglobin Sβ0 (HbSβ0) thalassemia living in low-middle–income settings; surveillance for developmental delay, cognitive impairments, and neurodevelopmental disorders in children; and use of magnetic resonance imaging of the brain without sedation to detect silent cerebral infarcts at least once in early-school-age children and once in adults with HbSS or HbSβ0 thalassemia. Individuals with SCD, their family members, and clinicians should become aware of and implement these recommendations to reduce the burden of CNS complications in children and adults with SCD.